Policies meant to restrict access to nicotine pouches are turning out to be counterproductive, especially for workers, whose access to tobacco alternatives is already constrained by time, location, and economic pressures. In New Brunswick, Canada, a construction worker’s story powerfully illustrates the human cost when safer options are forced off convenience shelves and buried behind pharmacy counters.
From Addiction to Opportunity
“I’m 32 … I was burning through a pack a day,” the worker shares. He describes trying every conventional route, patches, gum, hypnosis, but none anchored his cravings adequately. Then he discovered nicotine pouches: smoke-free, odorless, and easy to use on the job. He managed to quit cigarettes, sleep better, and feel healthier.
But soon after, Ottawa made nicotine pouches pharmacy-only items. Pharmacies close early or run out of stock. On job sites far from city centers, workers now must drive across towns just to find a pouch. Meanwhile, any corner store still sells cigarettes without a hurdle.
For many workers, this is more than inconvenience, it’s a barrier to quitting. Restricting access to safer products punishes people who likely have the least flexibility to adjust.
Who Is Disadvantaged?
White-collar professionals in cities may manage pharmacy hours and flexibility. But blue-collar workers, shift laborers, and remote site workers, these people have fewer options. Removing pouches from everyday retail channels forces them into a stark choice: either revert to cigarettes or face stackable time and cost burdens to access safer alternatives.
Policies framed as “for youth protection” can end up disproportionately hurting those most in need of quitting support. By moralizing nicotine, society treats addiction as sin rather than health, and in the process, sacrifices effectiveness.
What the Evidence Suggests
When safer alternatives become harder to access, smoking often returns. After San Francisco banned flavored vapes, high school cigarette use increased. U.S. states that clamp down on alternatives often see upticks in adult smoking.
On the other hand, markets that allow regulated access to oral nicotine products (like Sweden, where snus use is widespread) show dramatically lower rates of smoking and lung cancer. The Welsh experience, where pouch sales jumped nearly 92% in one year and users reported health gains, also supports the idea: when safer products are accessible, many smokers willingly switch.
These real-world signals should guide policy, not ideology or moral panic.
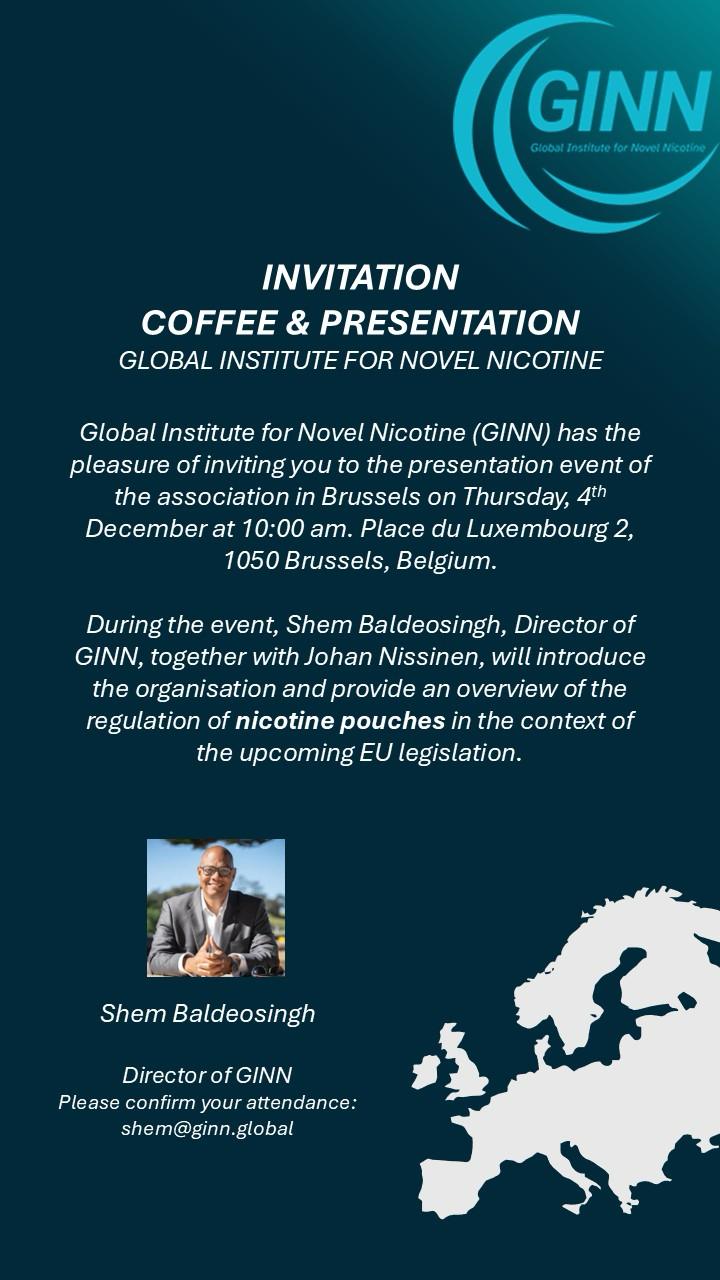
GINN’s Perspective
At GINN, public health should prioritize outcomes over optics. Nicotine pouches are not risk-free, but they are far safer than combustion. When used as a harm reduction tool, they offer a bridge for smokers who can’t or won’t quit nicotine altogether.
Restrictive policies that limit access to safer alternatives undermine public health goals. Every barrier we erect (pharmacy-only, limited supply, excessive regulation) is one more obstacle in someone’s path to quitting cigarettes.
Regulation should be smart: protect youth, ensure quality and availability, but don’t penalize those trying to make a healthier choice. Nicotine is addictive, but combustion is deadly. Let’s not make quitting harder under the guise of protection.